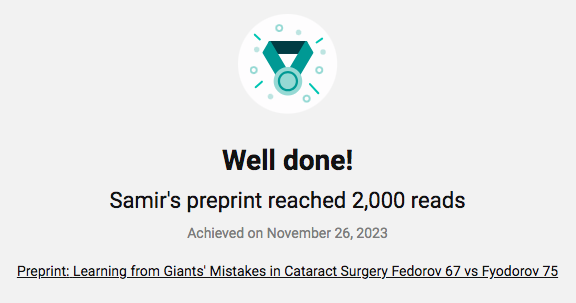
 Congratulations to Dr. Samir Sayegh on the recent announcement that his popular Research Gate preprint article reached 2,000 reads on November 26, 2023. Learning from Giants' Mistakes in Cataract Surgery Fedorov 67 vs Fyodorov 75 investigates one of the most influential papers in the history of cataract surgery. So called third and fourth generation intraocular lens calculation formulas implemented to this day are based on it. Dr. Sayegh shows that the actual expression given in the 1967 article is incorrect and was subsequently corrected by Fedorov and colleagues in 1975. He also shows the source of error and comments on implications for modern day intraocular power calculations for cataract surgery. Click
0 Comments
June is Cataract Awareness Month.  This month-long campaign aims to shine a spotlight on cataracts, a leading cause of vision impairment worldwide. Dennis Sherlin is a remarkable individual who faced a challenging battle with cataracts that left him alone, unemployed, and at an all-time low having lost his much-valued independence. Thanks to the dedicated efforts of Dr. Levenson and the transformative work of Operation Sight, Dennis' vision has been restored, enabling him to live life to the fullest once again. Click here to learn about how to become an ASCRS volunteer, or here to donate to the association. Careful biometry and corneal health are as important as choice of formula.  Dr. Samir Sayegh Dr. Samir Sayegh Review of Ophthalmology | January 2017 | Kristine Brennan, Senior Associate Editor Dr. Harold Ridley (1906-2001), who implanted the first intraocular lens in 1949, lived to see cataract surgery evolve into a true refractive procedure, undergoing IOL implantations himself in 1989 and 1990. Today, outcomes within half a diopter or less of target are attainable in most normal eyes, but some cases continue to present challenges. This article provides insights from seasoned cataract surgeons about how to maximize your outcomes and includes brief discussions of specific types of challenging eyes. Preop Workup is Critical “I can have a long eye, a short eye or a post-LASIK eye, but the most im- portant thing I do is give them all the same thorough preoperative workup,” emphasizes P. Dee Stephenson, MD, FACS, president of the American College of Eye Surgeons, associate professor at University of South Florida College of Medicine in Tampa and CEO/CFO of Stephenson Eye Associates. “I use the IOLMaster 700, the Cassini and the iTrace on every patient. I also do an OCT of the macula to make sure there is no pathology.” Samir Sayegh, MD, PhD, FACS, of the Eye Center in Champaign, Illinois, also considers a meticulous workup fundamental to a good refractive outcome. “We have a routine that applies to all eyes identified as being particularly exceptional,” he says. “We do a lot of repeat testing. We do partial coherence interferometry using the IOLMaster for axial length, and we do ultrasound. We do both every time, for every patient. For the measurement of the K value, we use at least three methods. Another thing we do is OCT of the retina for all patients. We also do pachymetry on all patients.” Dr. Sayegh says these measures help to reveal any pathology ahead of time. “Everybody having cataract surgery will get OCT, and they will get evaluation of the thickness of the cornea, so that if there is underlying Fuchs’ or anything that would be an issue at the time of surgery, we can take extra care with the eye. If there’s anything that would show up later, in the postop results, we also want to know ahead of time.” As IOL implantation inches closer to the long-term goal of emmetropia, surgeons implant challenging eyes with a more immediate goal: patient satisfaction and well-being. “You can plan all you want,” says Dr. Stephenson, “but sometimes there are surprises, and you have to look at the gestalt of the situation and make a decision that you think will be best for the patient.” Click here to read the entire article. Click here to view the Custom IOL Calculator that helps surgeons navigate lens choice. This new post shares a 2010 article on the unfinished stories of Intraocular Lenses.  With the availability of toric (astigmatism correcting) IOLs (intraocular lenses) to be used for cataract surgery, the best methods of using them are rapidly developing. In this context, we have recently obtained a patent about methods for optimally using these lenses and improve the results and visual performance for our patients. Some technical results can be consulted at USPTO.gov. Note: Previous work has been presented at the University of Illinois (UIUC), and elsewhere. Learning from Giants' Mistakes in Cataract Surgery Fedorov 67 vs Fyodorov 75 Samir I Sayegh, MD, PhD, FACS, FAAO, FASRS Click here to view the paper. Abstract
One of the most influential papers in the history of cataract surgery is Fedorov and Kolinko’s 1967 paper. All so called third and fourth generation intraocular lens calculation formulas implemented to this day are based on it. We show that the actual expression given in the 1967 article is incorrect and was subsequently corrected by Fedorov and colleagues in 1975. We show the source of error and comment on implications for modern day intraocular power calculations for cataract surgery. Introduction Slava Fedorov’s contributions to Ophthalmology are profound and lasting. In a paper with Albina Kolinko in 1967 they attempted a rational theoretical approach to the computation of intraocular lens (IOL) power based on biometry of the patient’s eye1. The paper was written in Russian and was followed by a few similar attempts by mainly European ophthalmologists. In 1975, together with Galin and Linksz, Fedorov (Fyodorov) contributed a similar article and computation to the English literature2. This made the approach more accessible to a wider readership and was followed by the (re)introduction of regression methods exemplified by SRK3,4 and somewhat later, by a realization that theoretical methods were foundational and need be adopted albeit with a grain of tweaking! This is represented by some of the major “third generation” or “vergence based” formulas such as Holladay1, SRKT and HofferQ5,6,7, all of which cite at least one of the Fyodorov and colleague’s papers and are in turn some of the most cited and implemented papers in the IOL power calculation literature. To our knowledge, there is no systematic comparison that has been attempted between the 1967 and 1975 versions of Fedorov and colleagues’ articles. In fact, a number of papers have cited both the 1967 and 1975 articles without mention of any discrepancy4,6,8. Others will cite only one9 or the other3,10,11. Some will mention a date and cite the article from the other date12. Yet others, surprisingly, cite neither13. In the present work we start by a direct comparison of the key formulas and their differences including numeric estimates and clinical implications. We follow with an analysis of the original sources and the sources of errors and draw conclusions as to lessons to be learned.  To address the global threat posed by diabetes, World Diabetes Day was established with the support of the World Health Organization (WHO) by the International Diabetes Federation in 1991. This date marks the birthday of Dr. Fredrick Banting, a co-discoverer of insulin. The 2022 theme is Access to Diabetes Care. One in 10 adults is living with diabetes and according to the WHO, close to 1 million are blind due to diabetic retinopathy. As the number of people with diabetes continues to rise, particularly in low- and middle-income countries, so too does the need for access to high-quality diabetes eye care. The ICO is in Official Relations with the WHO and promotes the key role of the ophthalmology community and those they work with in realizing the targets to increase eye-care coverage around the world. Free Online Low Vision Seminars The AFB (American Foundation for the Blind) recently referenced a report from Vision Serve Alliance that says only 3% of those who could benefit from low vision care actually get that care. The reasons vary, but among them are the reluctance, difficulty or inability of patients to go to a low vision practitioner due to the pandemic, distance or transportation issues. With Eschenbach’s telelowvision program, you can overcome all of those obstacles and reach those patients by conducting a virtual appointment and provide them the care they need! Would you like to know more about Low Vision without the hassles and costs of traveling to a conference? Eschenbach Optik of America provides free webinars on a variety of Low Vision topics that you can view and listen!
Wednesday, November 16, 2022 at 3pm Eastern, "Pediatric Low Vision: Determining which strategies and devices work best for your pediatric patients!"
Speaker: Dr. Thomas Porter, Director of Low Vision Services, Saint Louis University, Department of Ophthalmology. Approved for ACVREP credit. Click here to register. … and where in the world is Dr. Sayegh? So much is a part of our Eye Center family’s eye-centered world. From cutting edge research and world-wide presentations to the concerns and issues faced by our clients (and clients-to-be!). Here is where you will find the latest and greatest, and as always, if you have a concern or question, don’t hesitate to call and ask. We want for you the best vision your eyes can have!
Eye Center offices are conveniently located in Illinois and Indiana. Visit with us at a convenient Eye Center clinic located near you in Champaign, Chicago, Danville, and Mattoon, Illinois, and in Terre Haute, Indiana. We look forward to serving you.
|
AuthorEye Center Marketing Team Archives
November 2023
Categories |
Copyright ©2022, The Eye Center. All rights reserved.



 RSS Feed
RSS Feed